I. Mancini1, S. Riva2-3, A. Maino2,4, B. Ferrari2, A. Artoni2 and F. Peyvandi1,2
1Università degli Studi di Milano, Department of Pathophysiology and Transplantation, and Fondazione Luigi Villa, Milan, Italy; 2Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Angelo Bianchi Bonomi Hemophilia and Thrombosis Center, Milan, Italy; 3St Mary’s University, Twickenham, London, UK; 4Azienda Provinciale per i Servizi Sanitari, Internal Medicine Unit, Trento, Italy
BACKGROUND
- Acquired thrombotic thrombocytopenic purpura (TTP) is a rare multisystem microangiopathy with fluctuating signs and symptoms, typically of the nervous system, caused by the immune-mediated severe deficiency of the von Willebrand factor-cleaving protease ADAMTS13.1
- Despite the achievement of hematological remission, survivors of acute TTP may report persisting neurological impairment (e.g., difficulties with memory, headache, loss of concentration and endurance) that affects their quality of life.2-7
AIM OF THE STUDY
- To assess long-term neuropsychological consequences, emotional wellbeing and Health-related Quality of Life (HrQoL) in survivors of acute acquired TTP.
PATIENTS AND METHODS
- We performed a cross-sectional study of 35 patients with acquired TTP (25 non-relapsing and 10 relapsing TTP) regularly followed at our out-patient clinic of thrombotic microangiopathies between December 2015 and October 2016.
- Inclusion criteria: (a) diagnosis of acquired TTP;1 (b) 18 years of age or older at the time of enrolment; (c) adequate Italian language for the purpose of a valid psychometric testing.
- Exclusion criteria: (a) presence of severe neurological or psychiatric diseases before the onset of TTP; (b) drug or alcohol-abuse possibly impacting on quality of life and neuropsychological tests.
RESULTS
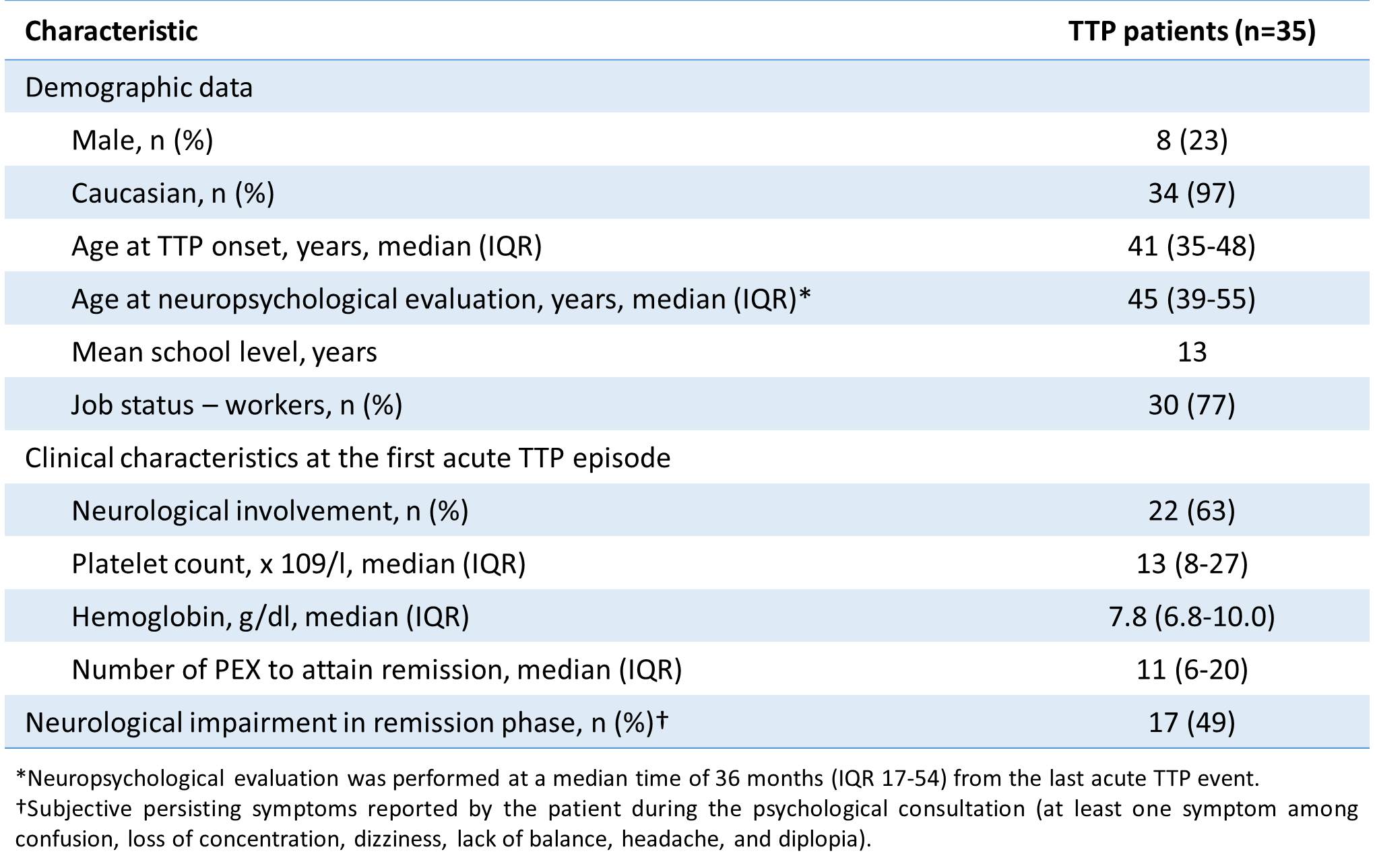
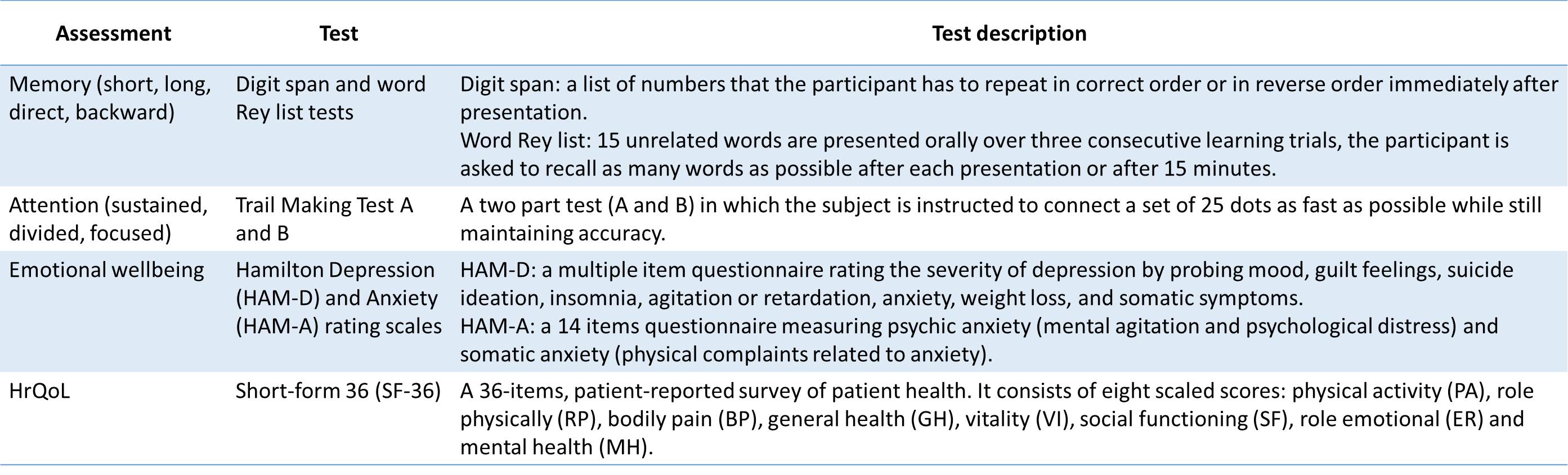
Table 1. Demographic and clinical characteristics of 35 TTP patients included in the study.
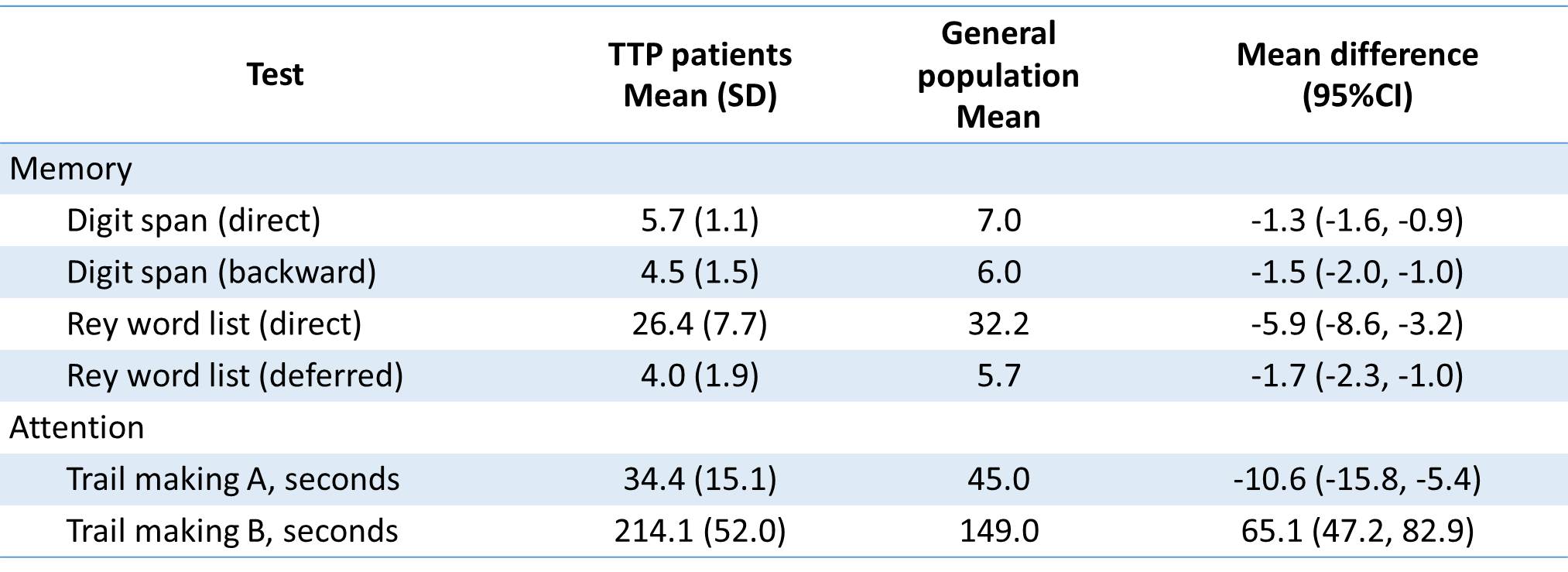
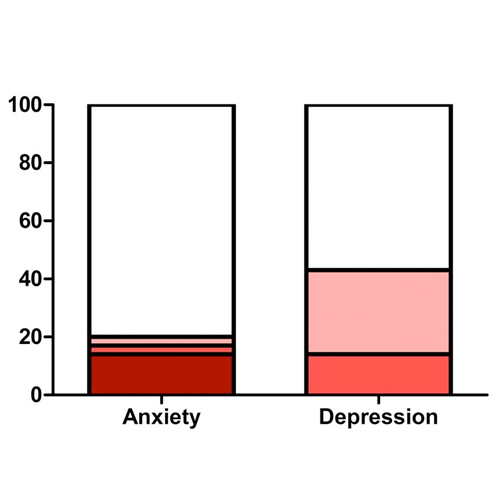
Table 2. Neuropsychological assessment revealed lower scores in tests of direct, indirect, deferred memory and attention compared with the general population.
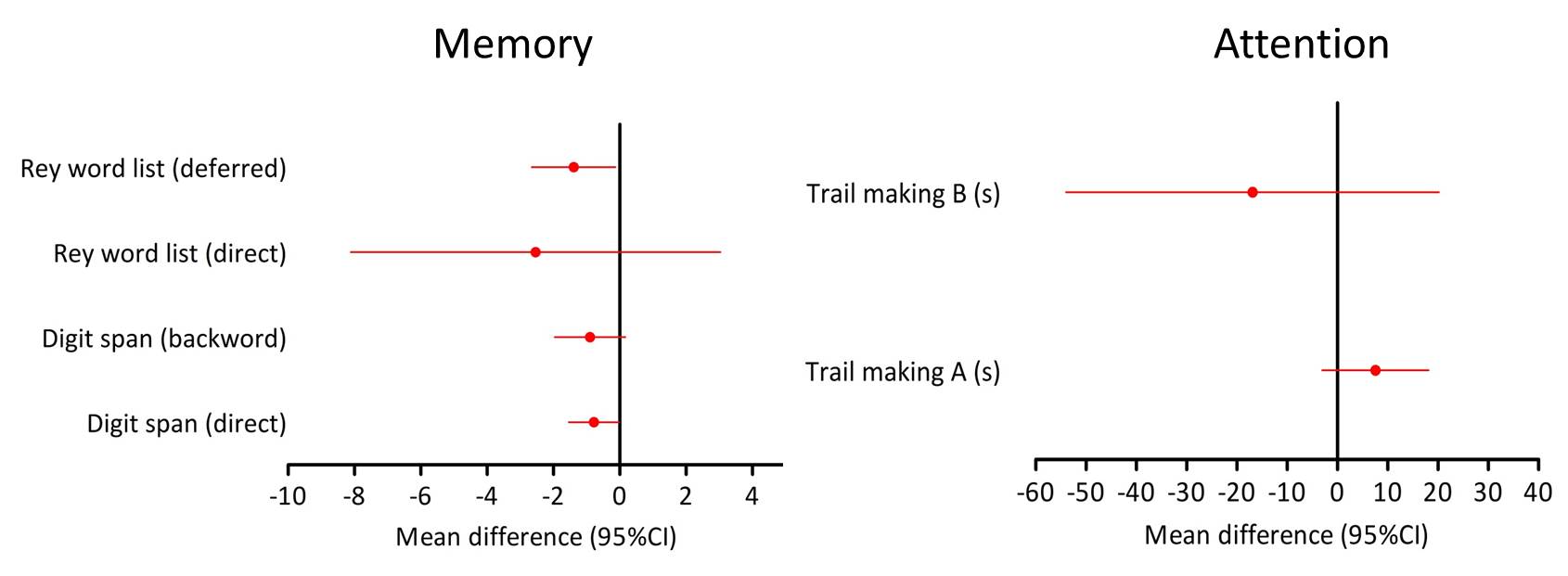
Figure 1. Patients with neurological manifestations at the first acute acquired TTP episode had higher impairment of memory domains compared with patient without acute neurological signs.
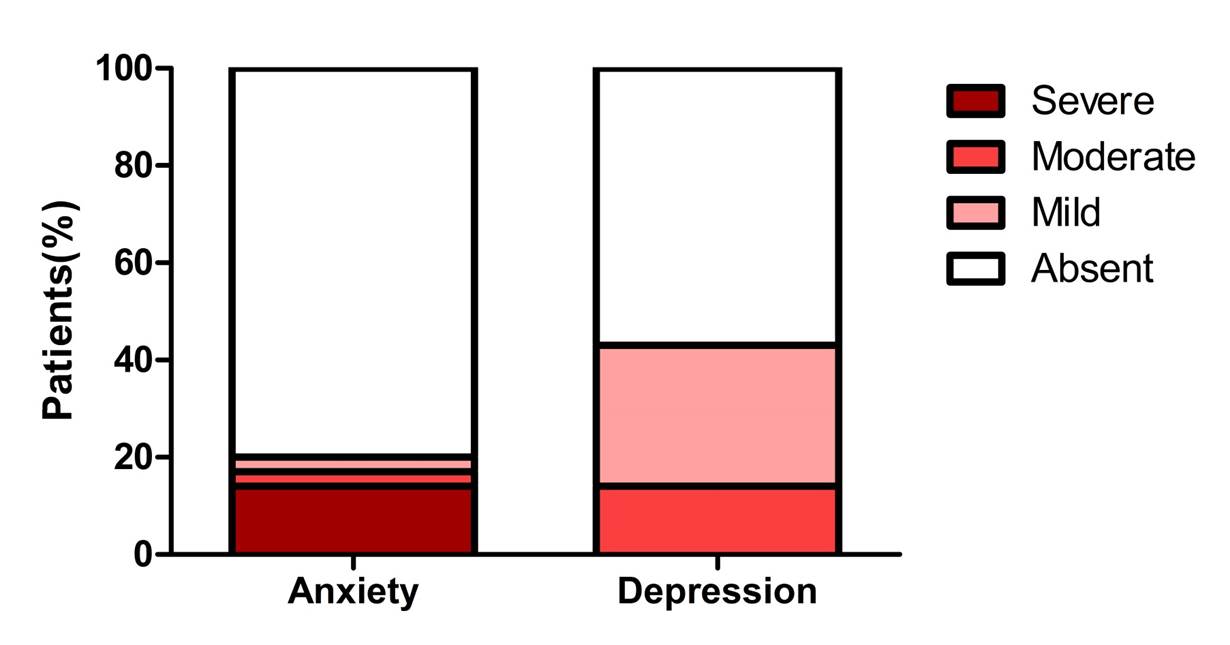
Figure 2. Clinical anxiety and depression was detected in 7 (20%) and 15 (43%) patients, respectively.
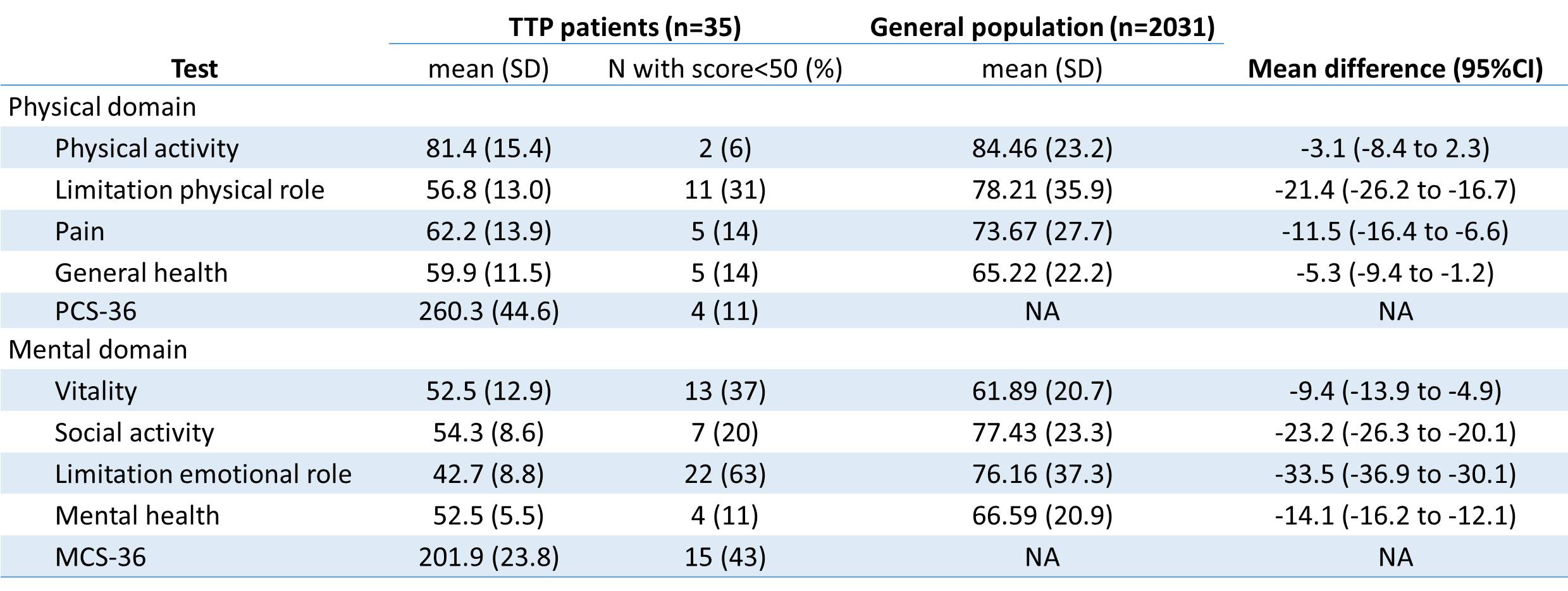
Table 3. HrQoL of acquired TTP patients was lower than the Italian general population, with mental domains more impacted than physical domains.
CONCLUSIONS
- Survivors of acute acquired TTP showed compromised memory and attentional functions, persisting anxiety/depression and a reduced quality of life perception.
- TTP patients with neurological involvement at the first acute episode seem to be at higher risk of developing memory dysfunction.
- Psychological assessment should be considered in routine clinical practice as it can help identifying cognitive or emotional abnormalities with important impact in every-day life.
- Longitudinal studies are required to monitor these dysfunctions over the time.
REFERENCES
- Scully M, Hunt BJ, Benjamin S, Liesner R, Rose P, Peyvandi F, Cheung B, Machin SJ; British Committee for Standards in Haematology. Guidelines on the diagnosis and management of thrombotic thrombocytopenic purpura and other thrombotic microangiopathies. Br J Haematol 2012; 158:323-335.
- Lewis QF, Lanneau MS, Mathias SD, Terrell DR, Vesely SK, George JN. Long-term deficits in health-related quality of life following recovery from thrombotic thrombocytopenic purpura. Transfusion 2009; 49:118-124.
- Kennedy KA, Lewis QF, Scott JG, et al. Cognitive deficits after recovery from thrombotic thrombo- cytopenic purpura. Transfusion 2009; 49(6):1092-1101.
- Han B, Page EE, Stewart LM, Deford CC, Scott JG, Schwartz LH, Perdue JJ, Terrell DR, Vesely SK, George JN. Depression and cognitive impairment following recovery from thrombotic thrombocytopenic purpura. Am J Hematol 2015; 90:709-14.
- Falter T, Schmitt V, Herold S, Weyer V, von Auer C, Wagner S, Hefner G, Beutel M, Lackner K, Lämmle B, Scharrer I. Depression and cognitive deficits as long-term consequences of thrombotic thrombocytopenic purpura. Transfusion 2017; 57:1152-1162.
- Chaturvedi S, Oluwole O, Cataland S, McCrae KR. Post-traumatic stress disorder and depression in survivors of thrombotic thrombocytopenic purpura. Thromb Res 2017; 151:51-56.
- Cataland SR, Scully MA, Paskavitz J, Maruff P, Witkoff L, Jin M, Uva N,Gilbert JC, Wu HM. Evidence of persistent neurologic injury following thrombotic thrombocytopenic purpura. Am J Hematol 2011; 86:87-90.